

“Improving compliance” expresses submission to a higher authority, and may cause tension in OR.įor this study we compated several previous models after founding Odgen criticizing the socio-cognition models in strategies to improve recommendation adherence. “Compliance” implies passive obedience or “giving in” to a mandate its use may reduce internal motivation and ownership of behavior. They found out that the terms used revealed the IC-strategy behind the program. They reported wide use of traditional components of the HBM: the personal susceptibility to illness severity of it the benefits of recommended action/behavior and the existence of psychological barriers such as cost, convenience, pain and embarrasment. Kretzer and Larson compared several models with similar constructs used in improving IC-practices. The concept of “compliance” was adopted from the Health Belief Model (HBM) originally developed to explain the use of health services and preventive health behavior of the patient. When improving the performance of AP it is useful to understand also the historical concepts and methods used in assessment of the IP.

#THE PRINCIPLES OF ASEPSIS PROFESSIONAL#
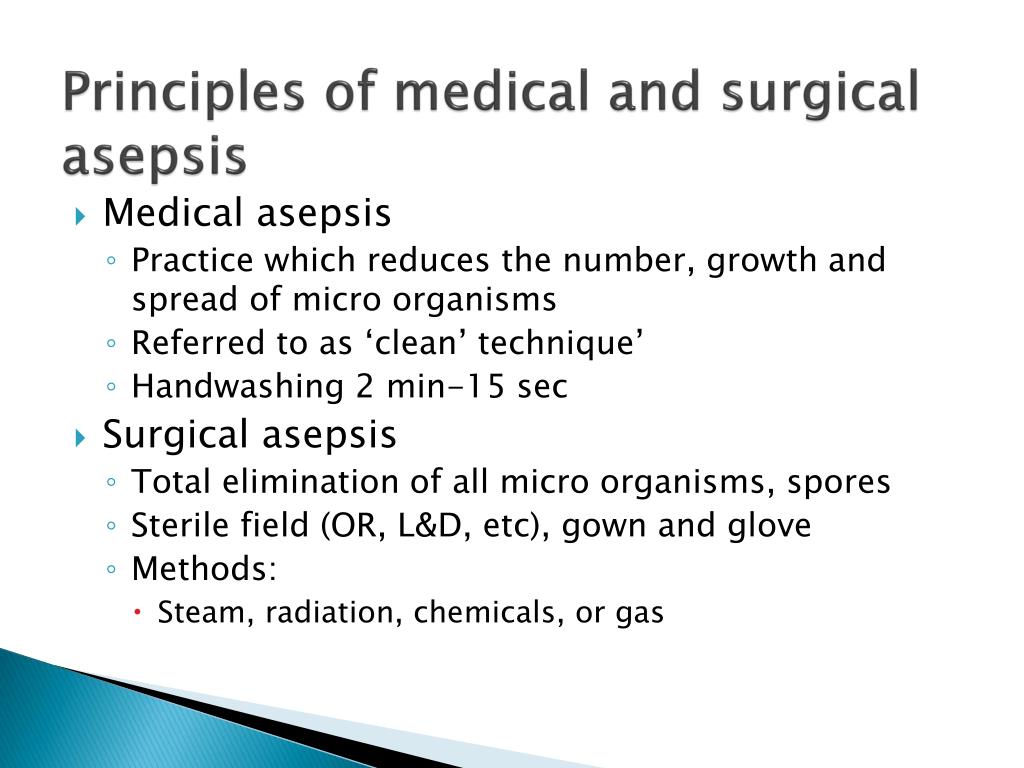
In this study we used the term “AP-adherence” when measuring the professional commitment to AP-recommendations. Breaks in AP was reported due to human behavior, lack of compliance with recommendations or adherence to infection control (IC)-procedures. When assessing surgical integrity, varying adherence of OR-nurses to AP-principles was reported and contaminations of sterile fields were observed. They are expected to be experts in the performance of perioperative AP to maintain surgical integrity and protect the sterile operating fields. In SSI-prevention the role of operating room (OR) nurses is valued important. In improving perioperative aseptic practice (AP) understanding of human behavior is beneficial. When the staff doesn’t apply precautions the behavioral and culture change is required. In the performance of these simple and low-cost IP-interventions staff accountability is essential. Appropriate hand hygiene and correct application of precautions during invasive procedures are key components in IP. Also WHO considers the promotion of protective measures and best practices key priorities in reducinge the burden of HCAI. One of their goals is to influence and facilitate legistative, accreditation, and regulatory agenda for infection prevention (IP) with consumers, policy-makers, health care leaders, and perssonnel.
The Association for Profesionals in Infection Control (APIC) has published a program to eliminate HCAIs. The most common HCAIs were SSI (24.3%) and pneumonia (24.3%) with estimated numbers of 157 500 each.
In 2011 in United States 4% of acute care inpatients had at least one HCAI. In developed countries SSI follows after urinary tract infections and the SSI-rates vary between 1.3 and 5.2%. The rates are varying from 1.2 to 23.6 infections per 100 surgical procedures. In low- and middle income countries surgical site infection (SSI) is the most frequent type of HAI. In USA, approxymately 99 000 deaths in 2002 and annual economic impact at approxymately US$ 6.5 billion in 2004, were attributed to HCAIs. In Europe annual financial losses are estimated at approxymately € 7 billion every year including direct costs only. For the health-care system HCAIs imply increased resistance to antimicrobials, and massive additional financial costs. The impact of HCAI implies prolonged hospital stay, long term disability, and excess deaths for the patients, and increased costs for the families. IntroductionĪccording to World Health Organization (WHO) health care associted infections (HCAI) are the most frequent adrverse event of patients while obtaining care. Identifying the reasoning for recommendation- adherence it may be possible to improve outcomes of infection prevention programs. The follow-up study among nurses only revealed lack of interest and need to study more the recommendation-adherence of nurses. There were differences in reasoning between nurses and physicians in the pilot study. A survey among OR-personnel revealed Situation-sensitivity, Reference-sensitivity, Ethical-sensitivity, and Infection-sensitivity factors for self-reported reasoning for adherence to aseptic practice recommendations. It is economically useful and ethical to improve surgical aseptic practice.


 0 kommentar(er)
0 kommentar(er)
